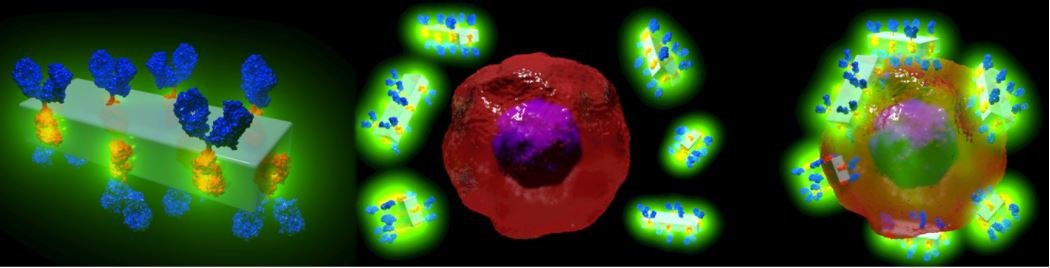
It sounds like the stuff of science fiction: a man-made crystal that can be attached to antibodies and then supercharge them with potent drugs or imaging agents (world-first antibody-drug delivery system) that can seek out diseased cells with the highest precision, resulting in fewer adverse effects for the patient.
However, that is precisely what researchers from the Australian Centre for Blood Diseases at Monash University in collaboration with the TU Graz (Austria) have developed: the world’s first (world-first antibody-drug delivery system) metal-organic framework (MOFs) that has the potential to fast-track potent new therapies for cancer, cardiovascular and autoimmune diseases.
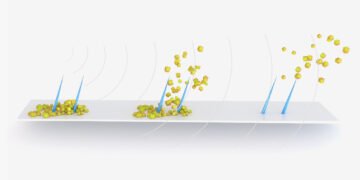
The in vitro study showed that when MOF antibody crystals bind to their target cancer cells and if exposed to the low pH in the cells, they break down, delivering the drugs directly and solely to the desired area.
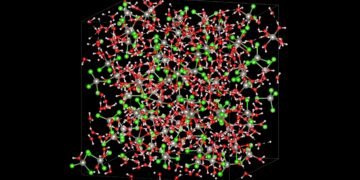
The metal-organic framework, a mixture of metal (zinc) and carbonate ions, and a small organic molecule (an imidazole, a colourless solid compound that is soluble in water) not only keeps the payload attached to the antibody but can also acts as a reservoir of personalised therapeutics. This is a benefit with the potential to become a new medical tool to target specific diseases with customised drugs and optimised doses.
The findings are now published in the world-leading journal Advanced Materials.
Co-senior author Professor Christoph Hagemeyer, Head of the NanoBiotechnology Laboratory at the Australian Centre for Blood Diseases, Monash University, says while more funding is needed to take the research into the next phase and to patients, the new method is cheaper, faster and more versatile than anything available currently.
“The method offers the opportunity to personalise treatment and given the precision possible, may eventually change the current dosage needed for patients, resulting in fewer side effects and making treatments cheaper,” said Professor Hagemeyer.
Co-first author Dr Karen Alt, Head of the NanoTheranostics Laboratory at the Australian Centre for Blood Diseases, Monash University, says: “With just 0.01 per cent of chemotherapy currently reaching the cancer tissue, this revolutionary new method can boost the potency of the drugs reaching their target.
“With over 80 different monoclonal antibodies approved for clinical use, this approach has enormous potential to improve these antibodies for the targeted delivery of diagnostic agents and therapeutic drugs. The goal is that ultimately the clinical translation of this technology will improve the quality of life for patients suffering from serious diseases,” said Dr Alt.