By Dr Arti Goel
The author is Assistant Professor with Amity Institute of Microbial Biotechnology, Amity University, Noida
Nanotechnology is the creation of useful materials, devices, and synthesis used to manipulate matter at an incredibly small scale—between 1 and 100 nm. Although “nanotechnology” has been an academic and media buzzword for several years, the federal government and private investors are now backing a host of initiatives with huge sums. Most current anticancer agents do not greatly differentiate between cancerous and normal cells, leading to systemic toxicity and adverse effects. This greatly limits the maximum allowable dose of the drug.
In addition, rapid elimination and widespread distribution into targeted organs and tissues requires the administration of a drug in large quantities, which is not economical and often results in undesirable toxicity. Several programs have supported research on novel nanodevices capable of detecting cancer at its premalignant stage, locating cancerous tissue within the body, delivering antineoplastic drugs to the cancer cells, and determining if these cells are being killed by the drugs. Nanocrystals and other nanoparticles have been receiving a lot of attention recently and their utilisation in cancer therapeutics is becoming a growing industry.
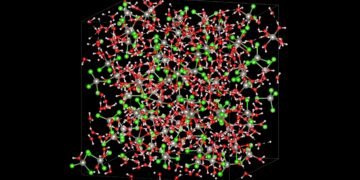
Cancer nanotechnology is an interdisciplinary area of research in science, engineering, and medicine with broad applications for molecular imaging, molecular diagnosis, and targeted therapy. The basic rationale is that nanometer-sized particles, such as semiconductor quantum dots and iron oxide nanocrystals, have optical, magnetic, or structural properties that are not available from molecules or bulk solids.
When linked with tumor targeting ligands such as monoclonal antibodies, peptides, or small molecules, these nanoparticles can be used to target tumor antigens (biomarkers) as well as tumor vasculatures with high affinity and specificity. In the mesoscopic size range of 5-100 nm diameter, nanoparticles also have large surface areas and functional groups for conjugating to multiple diagnostic (for example optical, radioisotopic, or magnetic) and therapeutic (like anticancer) agents.
Recent advances have led to bioaffinity nanoparticle probes for molecular and cellular imaging, targeted nanoparticle drugs for cancer therapy, and integrated nanodevices for early cancer detection and screening. These developments raise exciting opportunities for personalised oncology in which genetic and protein biomarkers are used to diagnose and treat cancer based on the molecular profiles of individual patients.
Physiologic and Biologic Characteristics of Nanoparticles
In chemotherapy, pharmacologically active cancer drugs reach the tumor tissue with poor specificity and dose-limiting toxicity. Conventional drug delivery methods include oral and IV routes. There are several disadvantages to these methods; for example, oral administration of tablets or capsules could result in disorderly pharmacokinetics due to the exposure of these agents to the metabolic pathways of the body. This can result in larger than necessary doses being administered, which can further cause increased toxicity.
The traditional IV routes are often even more problematic. The specificity of some conventional IV drugs is low, resulting in harmful effects to healthy tissues. Nanoparticle drug delivery, using biodegradable polymers, provides a more efficient, less harmful solution to overcome some of these problems.
It was in 1975 that Ringdorf proposed a polymer-drug conjugate model that could enhance the delivery of an anticancer model. He proposed that the pharmacologic properties of a polymer-drug conjugate model could be manipulated by changing the physical and chemical properties of the polymer. For example, an insoluble drug can be made water-soluble by introducing solubilising moieties into the polymer, thereby improving its bioavailability and biodegradability.
Cancer is caused by damage of genes which control the growth and division of cells. Genes carry the instructions for basic functions of cells. Cancerous cell need blood supply to grow. A hormone like molecule causes nearby blood vessel to grow towards the cell to supply the oxygen and other nutrients. Cancer can be cured by rectifying the damaging mechanism of the genes or by stopping the blood supply to the cells or by destroying it. Detection/diagnose is possible by confirming the growth of the cells.
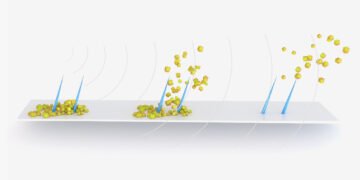
Scientists and researchers hope that nanotechnology can be used to create therapeutic agents that target specific cells and deliver the toxin in a controlled, time-release manner. The basic aim is to create single agents that are able to both detect cancer and deliver treatment. The nanoparticles will circulate through the body, detect cancer-associated molecular changes, assist with imaging release a therapeutic agent and then monitor the effectiveness of the intervention.
The use of nanotechnology in cancer treatment offers some exciting possibilities, including the possibility of destroying cancer tumors with minimal damage to healthy tissue and organs, as well as the detection and elimination of cancer cells before they form tumors.
Nanotechnology in Cancer Detection
Nanoparticles (NP) are of a few of nm and the cells are of the size of few microns. So, NP can enter inside the cells and can access the DNA molecules/Genes and, there is a possibility that the defect in the genes can be detected. DNA molecules can be detected in their incipient stage. This could be possible in vivo or in vitro.
Nanotechnology in Cancer Imaging
Application of nanotechnology to cancer imaging is subdivided into two main areas:
(1) Nanodetection for sensing protein and cancer cells
(2) Nanoparticle or nanovector formulation for high-contrast imaging.
Nanoparticles have been successfully used to selectively tag a wide range of medically important targets, including bacteria, biomarkers and individual molecules such as proteins and DNA. Nanoparticle devices are currently being developed for the early detection of cancer cells in body fluids such as blood and serum. Capturing circulating tumor cells is of great interest and is currently included in the design of large adjuvant and neo-adjuvant clinical trials.
Current systems are limited in their ability to accurately select and collect sufficient numbers of these cancer cells for analysis. On average there are only 1–2 cancer cells per
milliliter of blood. The nanoparticle devices being evaluated are conjugated with cancer-specific antibodies or ligands that may improve the yield of cancer cells captured. The field of imaging nanoparticles also offers fluorescent nanoplatforms on which targeting agents such as antibodies or ligands can be conjugated. It is possible to image a single cell or an entire organism in vivo.
Dual-mode nanoparticles can be imaged with MR and optical imaging. As the same particle is evaluated with different imaging modalities, accuracy is increased due to cross evaluation. More than 60 per cent of patients with breast, lung, colon, prostate, and ovarian cancer have hidden or overt metastatic colonies at the time of presentation. Currently MRI, positron emission tomography (PET), single photon emission tomography, and computed tomography (CT) are noninvasive imaging modalities used for cancer detection in humans.
Advances in nanotechnology may lead to a nanoparticle-based tumor-targeting contrast agent that will provide enhanced sensitivity and specificity for tumor imaging , enabling earlier detection of metastases. However, this could lead to over diagnosis and overtreatment in some instances, and this potential harmful effect should therefore be considered from the outset. Nanoparticle-enhanced MRI improved identification of lymph node metastasis in solid tumors. It was able to identify histologically positive nodes outside the usual field of resection, effectively “upstaging” a proportion of cancers that would have otherwise been identified as node negative.
Nanotechnology in Cancer Treatment
Certain nanoparticles can be designed to absorb preferentially certain wave length of radiation and gets heated. Such a NP if enters in the cancerous cell will burn it if irradiated by suitable wavelength radiation. This is kind of the analogue of radiation therapy. As mentioned before, nanotechnology can be used to create therapeutic agents that target specific cells and deliver toxin to kill them. The NP will circulate through the body, detect cancer associated molecular changes, assist with imaging release a therapeutic agent and then monitor the effectiveness of the intervention.
Advantages and Challenges of Nanotechnology in Cancer therapy
Nanotechnology has many advantages in cancer therapy. With small size, nanotechnology platforms can enter tumor vasculature via EPR. Besides, functionalisation with hydrophilic polymer/oligomer can offer a long circulation
Halflife and prolong the exposure time of tumor tissue to anticancer agents; whereas inclusion of tissue recognition residues, such as antibodies, lectins and ligands which are specific for cancer cells, can help nanotechnology platforms achieve tumor cell targeting. For overcoming MDR of cancer cells, a major challenge in effective cancer therapy, combinations of multifunctional nanotechnology platforms and other therapies have been developed and achieved significant successes.
However, there are still challenges to the development and application of nanotechnology platforms in cancer therapy, such as limited knowledge of the cancer cell physiology, small variety and poor functionalisation of medical nanomaterials, and deficiency of clinical evaluation criteria.
Nonetheless, with further advances in functionalisation base on thorough understanding of the physiological features of cancer cells, nanotechnology platforms hold the promise of essentially changing the practice of oncology, allowing easy and effective targeted therapies.
Further Reading
- McCarthy JR, Weissleder R (2008). Multifunctional magnetic nanoparticles for targeted imaging and therapy. Adv Drug Deliv Rev 60(11):1241–1251.
- Ferrari M (2005). Cancer nanotechnology: opportunities and challenges. Nat Rev Cancer 5(3):161–171.
- Medarova Z, Pham W, Farrar C, Petkova V, Moore A (2007). Invivo imaging of siRNA delivery and silencing in tumors. Nat Med 13(3):372–377.
- Hirsch LR, Gobin AM, Lowery AR, Tam F, Drezek RA, Halas NJ et al (2006). Metal nanoshells. Ann Biomed Eng 34(1):15–22.
- Hirsch LR, Stafford RJ, Bankson JA, Sershen SR, Rivera B, Price RE et al (2003). Nanoshell-mediated near-infrared thermal therapy of tumors under magnetic resonance guidance. Proc Natl Acad Sci USA 100(23):13549–13554.
- McCarthy JR, Kelly KA, Sun EY, Weissleder R (2007). Targeted delivery of multifunctional magnetic nanoparticles. Nanomed 2 (2):153–167.
- Dinh P, Sotiriou C, Piccart MJ (2007). The evolution of treatment strategies: aiming at the target. Breast 16(Suppl 2):S10–S16.
- Nie S, Xing Y, Kim GJ, Simons JW (2007). Nanotechnology applications in cancer. Annu Rev Biomed Eng 9:257–288.
- Kumar R, Roy I, Ohulchanskyy TY, Goswami LN, Bonoiu AC, Bergey EJ et al (2008). Covalently dye-linked, surface-controlled, and bioconjugated organically modified silica nanoparticles as targeted probes for optical imaging. ACS Nano 2(3):449–456.
- Menon U, Jacobs IJ (2000). Recent developments in ovarian cancer screening. Curr Opin Obstet Gynecol 12(1):39–42.
- Wang X, Yang L, Chen ZG, Shin DM (2008). Application of nanotechnology in cancer therapy and imaging. CA Cancer J Clin 58(2):97–110.
- Harisinghani MG, Barentsz J, Hahn PF, DesernoWM, Tabatabaei S, van deKaa CH et al (2003). Noninvasive detection of clinically occult lymph-node metastases in prostate cancer. N Engl J Med 348 (25):2491–2499.
- Harisinghani MG, Weissleder R (2004). Sensitive, noninvasive detection of lymph node metastases. PLoSMed 1(3):e66.
- Kim KY (2007). Nanotechnology platforms and physiological challenges for cancer therapeutics [J]. Nanomedicine, 3(2):103-110.
- Alivisatos A. (1996). Perspectives on the physical chemistry of semiconductor nanocrystals. J Phys Chem,100: 13226–39.
- Suntherland A (2002). Quantum dots as luminescent probes in biological systems. Curr Opin Solid State Mater Sci,6:36–370.
- Williams J, Lansdown R, Sweitzer R, et al (2003). Nanoparticle drug delivery system for intravenous delivery of topoisomerase inhibitors. J Control Release, 91:167–72.
- Leroux J-C, Allemann E, De Jaeghere F, Duelker E, Gurny R (1996). Biodegradable nanoparticles—From sustained release formulation to improved site specific drug delivery. J Control Release, 30: 339–50.