Nanoparticle containing mRNA shown to prevent and treat peanut allergy in mice. The technology developed by UCLA may provide a platform to fight other allergies and autoimmune diseases. Peanut allergy affects 1 in 50 children, and the most severe cases lead to a life-threatening immune reaction called anaphylactic shock.
Currently, there is only one approved treatment that reduces the severity of allergic reactions, and it takes months to start. A group of UCLA immunologists wants to change that.
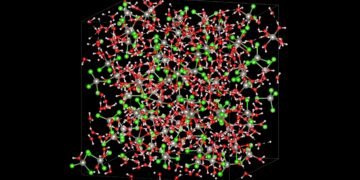
Taking inspiration from the COVID-19 vaccine and their own research into the disease, they developed a type of nanoparticle – as small as one billionth of a meter – that delivers mRNA into the liver of certain cells. These cells, in turn, teach the body’s natural defenses to accept peanut protein.
When tested on mice, the nanoparticle not only reversed peanut allergies, but also prevented them from developing. The study was published in the journal ACS Nano.
“As far as we can tell, mRNA has never been used for cancer,” said Dr. André Nel, co-author of the paper, UCLA Distinguished Professor of Medicine and director of research at the California NanoSystems Institute at UCLA said. “We have shown that our platform can work to make peanut butter cool, and we think it can do the same for other allergens, in food and medicine, and autoimmune diseases.”
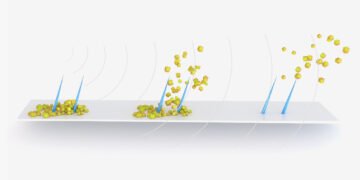
The researchers focused on the liver for two reasons: First, the organ is trained not to react to any challenge because foreign substances are used when all, including harmful substances. Second, the body contains cells called antigen-presenting cells, which pick up foreign proteins and train the immune system to cope with them instead of attacking them when detected.
This study builds on two earlier advances made by Nel and his colleagues. In 2021, they discovered that a nanoparticle that delivers a carefully selected fragment of a protein, called an epitope, to the liver reduced the symptoms of a dangerous egg allergy in mice. The following year, they discovered an epitope that reduced peanut allergy in mice when delivered to the liver via a nanoparticle. Because these epitopes leave out the part of the peanut or egg protein that causes allergies, they are expected to be safe as part of the treatment.
“If you are lucky enough to choose the right way, there is a protective mechanism that reduces the reaction with other fragments,” said Nel, who directs the Center for Environmental Implications of Nanotechnology at the University California, or CEIN. . “That way, you can take care of the whole series of epitopes that play a role in disease.”
The scientists improved their previous nanoparticle design by adding a sugar molecule to its surface that binds specifically to antigen-presenting cells. Using mRNA is another step forward.
In the improved nanoparticle, the researchers engineered a portion of the mRNA payload to encode a selected epitope or epitopes – in this case, a peanut protein fragment identified in previous studies – as an mRNA vaccine for SARS-CoV-2. All proteins are included. of the virus. The use of mRNA makes nanoparticle loading easier and eliminates the problem of including more than one epitope, an advantage that can be quickly expanded. For example, multiple epitopes may be needed to treat certain other allergies or multiple allergens.
To find out if their improved nanoparticle will prevent peanut allergies, the researchers gave it to six mice in two sessions, one week apart. Another group of six mice received a nanoparticle with the same mRNA as a payload, but without the targeted sugar on it; Another six rats received the enhanced nanoparticle but contained mRNA that did not code for any protein or epitope; and a third of the sixth group did not receive nanoparticles. Starting one week after the second treatment, they gave the mice crude peanut protein extracts to make them feel like peanuts. Another week later, they exposed the mice to peanut protein to induce anaphylactic shock.
Mice that had been treated with nanoparticle showed a mild signal compared to those who received nanoparticle without sugar, while strong signal means that the control group receives no treatment and the group that receives the nanoparticle targeted to the mRNA is is not a code.
The scientists repeated the experiment, changing the method that works so that the mice understand the peanut protein before they receive the nanoparticle. Also, the improved nanoparticle appeared better than a similar nanoparticle without targeted sugar, and both produced milder symptoms than the researchers found in mice that did not receive treatment or a nanoparticle with non-coding mRNA.
In two versions of the experiment, scientists measured the level of specific immune cells and some antibodies, enzymes and cytokines, which confirmed that the improved nanoparticle made the animals more tolerant to peanut protein.
Nel estimates that with the success of further laboratory studies, the nanoparticle could be in clinical trials within three years. (His lab will soon begin the design process necessary to test the peanut formula in clinical trials.) He added that replacing mRNAs that encode different epitopes opens up the possibility of nanoparticle preparation for other allergies and autoimmune diseases.
The team is investigating whether nanoparticles can be used to treat type 1 diabetes, a disease in which the immune system attacks the cells in the pancreas that allow the body to obtain energy from food. Other researchers have already identified important epitopes of proteins that trigger anti-diabetic attacks.
Source: UCLA