A New way to spot bacteria in fluids, new technological advances in old inkjet printers and AI-assisted imaging are making it faster and cheaper to detect bacteria in blood, feces and more.
Shine a laser on a drop of blood, nose or feces, and the bright light can be used to detect bacteria in the sample.
“We can detect not only the bacteria present, but more specifically the bacteria in the sample – E. coli, Staphylococcus, Streptococcus, Salmonella, anthrax, etc.,” said Jennifer Dionne, professor of science and technology and other things said. , courtesy of Stanford University Radio. “Each microbe has a unique optical fingerprint. It is like the genetic and proteomic code written in light.
Dionne is the lead author of a new study in the journal Nano Letters outlining a new method her team has developed that could lead to fast (almost instantaneous), cheap and accurate microbial analysis. which is almost any water for germs.
Traditional methods that are still used today can take hours or even days. TB cultures take 40 days, Dionne said. The new test can be done in minutes and promises better and faster disease diagnosis, better use of antibiotics, better nutrition, environmental monitoring and faster drug development, the group said.
Old dog, new trick
The breakthrough is not that the bacteria display these different fingerprints, a fact known for decades, but that the team was able to reveal these patterns in the middle of a blinding light displayed from each view.

“Not only does each type of bacteria exhibit unique light patterns, but almost every molecule or cell in a given sample does too,” first author Fareeha Safir said, a PhD student in Dionne’s lab. “The red blood cells, white blood cells, and other components of the sample send back their own signals, making it difficult, if not impossible, to distinguish between microbial species and the noise of other cells.”
One milliliter of blood – the size of a drop of water – can contain billions of cells, only a few of which can be microbes. The team needed to find a way to isolate and amplify the light reflected from the bacteria alone. In order to do this, they took many surprising scientific tangents, combining forty-year-old technology borrowed from computers – inkjet printers – and two critical technologies of our time – nanoparticles and intelligence.
“The key to isolating bacteria from other markers is to isolate cells in a small sample. We use the principle of inkjet printing to print thousands of tiny blood spots instead of interviewing one large sample,” says the researcher. Butrus “Pierre” Khuri-Yakub, an emeritus professor of electrical engineering at Stanford who helped develop the first inkjet printer in the 1980s.
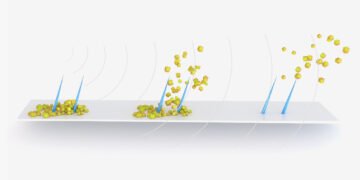
“But you can’t get a standard inkjet printer and add blood or feces,” Safir said. To avoid the challenge of handling live samples, the researchers modified the printer to apply the sample to paper using acoustic waves. Each drop of blood printed is only two trillionths of a liter in size, more than a billion times smaller than a drop of rain. At this scale, the water droplets are so small that they can contain only a dozen molecules. In addition, the researchers introduced the sample to a gold nanorod that binds to the bacteria, if present, and acts as antennae, attracting the laser light to the bacteria and amplifying the signal. body about 1,500 times its power is not strong.
Well separated and spread out, bacterial species appear like scientific fingerprints. The final part of the puzzle is to use machine learning to compare the spectrum reflected from each spot of printed water to see the signature of each bacteria in the sample.
“It’s a new solution that can save lives. We are now excited about a commercial opportunity that can help define the standard for virus detection and single-cell identification,” co-author Amr Saleh, a former postdoctoral researcher in Dionne’s lab and now a professor at Cairo University said.
Collaborator
This collaborative nature of the discipline is characteristic of Stanford’s tradition of scholars from seemingly disparate backgrounds bringing their diverse expertise to bear on long-standing problems of social impact.
The process originated from a lunch meeting at the campus cafe and, in 2017, was among the first recipients of a $3 million grant program distributed by the Catalyst for Collaborative Solutions from Stanford. Catalyst’s grants are intended to stimulate innovation and collaboration among Stanford researchers in high-reward areas such as health care, the environment, self-reliance, and security.
Although this method was developed and perfected using blood samples, Dionne also believes that it can be applied to other types of water and target cells beyond bacteria, such as testing cleanliness. more expensive than the current method.
Source: Stanford University.