New nanotechnology that accelerates the transition of stem cells into bone (Bone Formation Comes Down to the Nanowire) could transform regenerative medicine.
A nanotechnology platform developed by King Abdullah University of Science & Technology (KAUST) scientists could lead to new treatments for degenerative bone (Bone Formation Comes Down to the Nanowire) diseases.
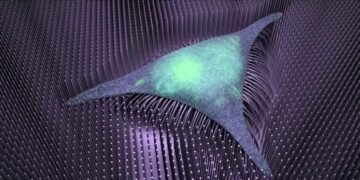
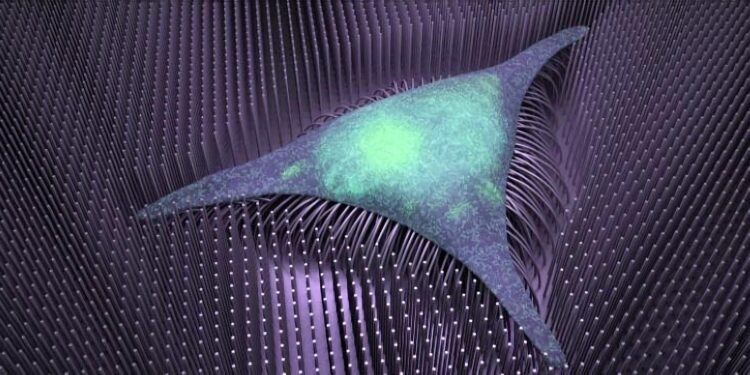
The technique relies on iron nanowires that bend in response to magnetic fields. Bone-forming stem cells grown on a mesh of these tiny wires get a kind of physical workout on the moving substrate. They subsequently grow into adult bone considerably quicker than in conventional culturing settings, with a differentiation protocol that lasts only a few days rather than a few weeks.
“This is a remarkable finding,” says Jasmeen Merzaban, associate Professor of bioscience. “We can achieve efficient bone cell formation in a shorter amount of time,” potentially paving the way for more efficient regeneration of bone. Merzaban co-led the study together with sensor scientist Jürgen Kosel and colleagues from their labs.
The scientists analyzed the bone-producing capability of their nanowire scaffold, both with and without magnetic signals. They patterned the tiny wires in an evenly spaced grid and then layered bone marrow-derived human mesenchymal stem cells (MSCs) on top. Each of the tiny wires is about the size of the tail-like appendage found on some bacteria.
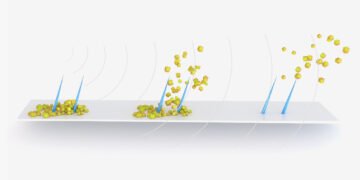
The researchers discovered that adding a low-frequency magnetic field greatly accelerated the process of bone development. Within two days of incubation under mechanical stimulation, genetic markers of bone development could be detected, while genes linked to stemness and self-renewal quickly became inactive. The scientists could also witness the cells rebuilding themselves to become more bone-like at a rapid rate under a microscope.
Next, the KAUST team plans to test its system in mouse models of degenerative bone disease, with the expectation that stem cell–seeded nanowire scaffolds can be safely implanted at sites of injury and promote tissue repair. An externally applied magnetic field would be used to speed the healing process.
Study author Jose Efrain Perez, a former Ph.D. student in Kosel’s lab, also sees potential applications in other disease settings. As he points out: “Varying the matrix stiffness by increasing or decreasing nanowire length and diameter could promote differential responses with MSCs.” Or they could use other types of stem cells to, for example, promote neuronal growth and brain repair after a stroke.
What’s more, Perez adds, “We could further customize the nanowire scaffold itself or the base material — for instance, by using different metals to exploit their magnetic responses or coating the nanowires with biomolecules for potential delivery upon cellular contact.”
For such a small technology, the possibilities are huge.