Technical advances allow particles to be placed deeper into biological tissues, which could aid in the diagnosis or monitoring of cancer (Fluorescent sensor – Provides unique insight inside living cells).
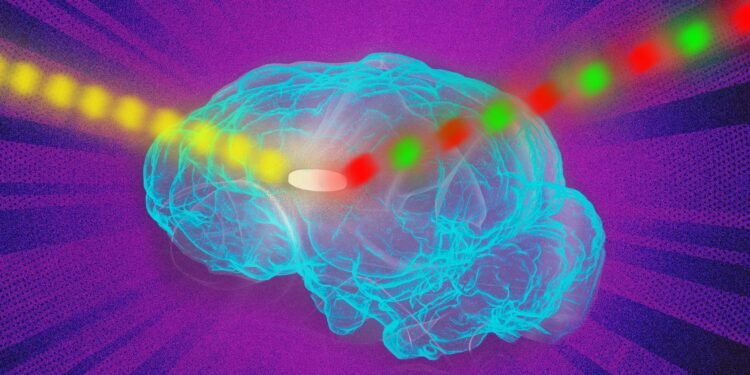
Fluorescent sensors, which can be used to label and image a wide variety of molecules, provide unique insights inside living cells. However, they can usually only be used in cells grown in a lab dish or in tissues near the surface of the body, because their signal is lost when implanted too deeply.
MIT engineers have now developed a solution to overcome this limitation. By using a new photonics technique they invented to excite any fluorescence sensor, they were able to dramatically improve the fluorescence signal. With this approach, the scientists demonstrated that they could implant sensors up to 5.5 centimeters (2.2 inches) deep into tissue and still pick up a strong signal.
According to the researchers, this type of technology could use fluorescent sensors to monitor specific molecules inside the brain or other deep tissues of the body, for medical diagnostic purposes or to monitor effects. of drugs. Researcher Volodymyr Koman at MIT and one of the lead authors of the new study. Naveed Bakh SM ’15, PhD ’20 is also the lead author of the paper, which was published May 30, 2022 in Nature Nanotechnology. Michael Strano, P. Dubbs Professor of Carbon Chemical Engineering at MIT, is the study’s lead author. Fluorescence improvement
Scientists use a variety of fluorescent sensors (Fluorescent sensor – Provides unique insight inside living cells), including quantum dots, carbon nanotubes and fluorescent proteins, to label molecules inside cells. The fluorescence of these sensors can be seen by shining a laser light at them. However, it does not work in dense, dense tissue or deep in tissue, because the tissue itself also emits fluorescent light. This light, called autofluorescence, drowns out the signal from the sensor.
“All tissues are autoluminescent, and that becomes a limiting factor,” says Koman. “As the sensor signal gets weaker and weaker, it is overtaken by tissue autofluorescence.”
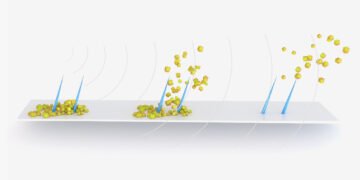
To overcome this limitation, the MIT team found a way to modulate the frequency of the fluorescent light emitted by the sensor so that it can be easily distinguished from tissue autofluorescence. Their technique, which they call Wavelength Inductive Frequency Filtering (WIFF), uses three lasers to produce a laser beam of oscillating wavelengths. When this oscillating beam is shined on the sensor, it causes the fluorescence emitted by the sensor to double in frequency. This makes it easy to distinguish the fluorescence signal from the background autofluorescence. Thanks to this system, the researchers were able to multiply more than 50 signal-to-noise ratios of the sensors. One possible application for this type of detection is monitoring the effectiveness of chemotherapy drugs. To demonstrate this potential, the researchers focused on glioblastoma, an aggressive type of brain cancer. Patients with this type of cancer often have surgery to remove as much of the tumor as possible and then receive the chemotherapy drug temozolomide (TMZ) to try to remove any remaining cancer cells.
This drug can have serious side effects and doesn’t work for all patients, so it would be helpful if you had a way to easily monitor if it’s working, says Strano. “We are working on technology to create tiny sensors that can be implanted near the tumor itself, which can give an indication of how much drug is going to the tumor and whether it is being metabolized. You can place a sensor near the tumor and check from outside the body how well the drug is working in the real environment of the tumor,” he said. When temozolomide enters the body, it breaks down into smaller compounds, including one known as AIC. The MIT team designed a sensor that can detect AIC and showed they could implant it up to 5.5 centimeters long into the brains of animals. They can read sensor signals even through the animal’s skull. Such sensors could also be designed to detect molecular markers of tumor cell death, such as reactive oxygen species. “Any Wavelength”
In addition to detecting TMZ activity, the researchers demonstrated that they can use WIFF to enhance signals from many other sensors, including the carbon nanotube-based sensor that Strano’s lab has developed previously developed to detect hydrogen peroxide, riboflavin, and ascorbic acid. “This technique works at any wavelength and can be used for any fluorescent sensor,” says Strano. “Because you have more signals now, you can implant a sensor at a depth in tissue that wasn’t possible before.”
For this study, the researchers used three lasers together to create an oscillating laser beam, but in future research they hope to use a tunable laser to signal generation and further technical improvements. This will become more possible as the prices of tunable lasers drop and they become faster, the researchers say. To make fluorescent sensors easier to use in human patients, researchers are working on sensors that are bio-resorbable, so they don’t need to be surgically removed.