Over the past 30 years, advances in early detection and treatment of cancer have helped reduce the overall death rate by more than 30%. However, pancreatic cancer remains difficult to treat. Only 1 in 9 people survive five years after being diagnosed, in part because this cancer is protected by preventive measures. Hoping for a breakthrough, UCLA researchers have developed a technology that delivers a combination therapy for pancreatic tumors (‘Glass bubble’ nanocarrier enhances efficacy of combination therapy for pancreatic cancer) using nanoparticles loaded with irinotecan, an approved chemotherapy and drug treatment for pancreatic cancer, and 3M-052, an experimental drug that can improving immune function and helping to fight against tumors.
In a study recently published in the journal ACS Nano, the research team showed that the combination administered at the same time was superior to the combination of its components in a mouse model of pancreatic cancer.
“In my opinion, invoking the immune system will make a big difference in providing the best treatment results for pancreatic cancer,” said corresponding author André Nel, Professor of Medicine and Researcher at California NanoSystems Institute of UCLA said. “That’s where I hope this discovery will take us.”
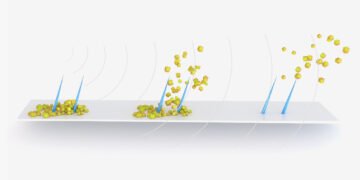
The nanocarrier used by the researchers was twice as effective against the tumors in preventing cancer metastasis and more than irinotecan without the nanocarrier or nanocarriers that deliver the two drugs independently. This combination therapy also attracted cancer-fighting cells to the tumor site and maintained long-term levels of the drug in the blood. There is no evidence of harmful effects.
In addition to inhibiting the growth of cancer cells, irinotecan sends dangerous signals to the dendritic cells of the immune system; these recruit killer T cells, which travel to the tumor to destroy cancer cells. But because dendritic cells often work well in patients with pancreatic cancer, 3M-052 provides additional support, helping them to recruit T cells that kill more effectively and at the site cancer in the lymph nodes.
Combination therapy for cancer is nothing new, but co-packing drugs together in a single nanocarrier has proven difficult. One nanocarrier delivers two for chemotherapy as approved by the Food and Drug Administration. However, for the past seven years, Nel’s laboratory has been developing a delivery system at the same time, and the results now provide more evidence that their new nanocarrier design allows the drug to work work in tandem better than if they are offered.
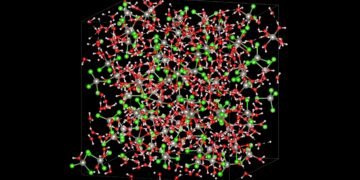
Most nanocarriers are composed of lipid molecules made of lipid-based materials, such as animal skin, with cavities where drugs can be concentrated. In this new device, a double layer of lipids surrounds the center of the silica glass bubble whose interior can be filled with irinotecan. In a clever twist, UCLA postdoctoral researcher and first author Lijia Luo discovered that the fatty tail of 3M-052 could be used to insert a second drug directly into these lipid layers.
The design of the adapter, which is so small, it would take 1,000 to expand the width of a human hair, helps to prevent drug poisoning and poisoning as the device penetrates into dangerous obstacles such as fibers Prevent pancreatic cancer and go to the tumor site. The glass bubble provides additional protection against leakage, allowing the carrier to deliver the irinotecan form to the tumor site, compared to other drug carriers.
The team will conduct additional preclinical studies to test their treatment in larger animal models and support quality control for large-scale production of their silica nanocarriers.
“It usually takes 10 to 20 years for new technological advances to come to market,” said Nel, who is also the founder and director of UCLA’s department of nanomedicine and director of the Center for Environmental Implications of Nanotechnology. University of California. “Nanocarriers have been around for almost 20 years. Although lipid-based nanocarriers lead the way, a silica carrier decorated with lipid layers has a good chance of accelerating the diagnosis and improving cancer immunotherapy.