Testing for malaria could become as simple as putting on a bandage.
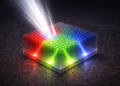
That’s the idea behind a platform developed by Rice University engineers who introduced a microneedle patch for rapid diagnostic testing that does not require extracting blood.
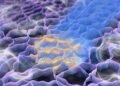
The device detailed in the Nature journal Microsystems and Nanoengineering (“Microneedle-based skin patch for blood-free rapid diagnostic testing”) draws upon protein biomarkers contained in dermal interstitial fluid, what people generally recognize as the fluid inside blisters but surrounds all of the cells in skin.
This fluid contains a multitude of biomarkers for various diseases, such as malaria, which can be used for rapid testing. The disposable patches could be programmed to detect other diseases, potentially including COVID-19, said mechanical engineer Peter Lillehoj of Rice’s Brown School of Engineering.
“In this paper, we focus on malaria detection because this project was funded by the Bill and Melinda Gates Foundation, and it’s a big priority for them,” said Lillehoj, who joined Rice in January as an associate professor of mechanical engineering. “But we can adapt this technology to detect other diseases for which biomarkers appear in interstitial fluid.”
The self-contained test developed by Lillehoj and lead author Xue Jiang, a Rice postdoctoral researcher, delivers a result in about 20 minutes and does not require medical expertise or any equipment.
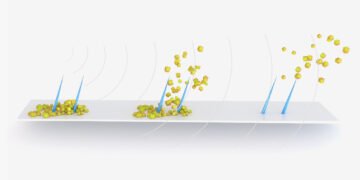
The sticky patch has 16 hollow microneedles in a 4-by-4 array on one side, coupled with an antibody-based lateral-flow test strip on the other. The antibodies react when they sense protein biomarkers for malaria and turn two readout lines on the strip’s exposed surface red. If the test is negative, only one line turns red.
The needles are treated to be hydrophilic — that is, attracted to water — so the fluid is drawn in and flows through to the test strip. Once the test is complete, the device can be removed like any bandage.
While both microneedles and antibody test strips have been extensively studied, Lillehoj said his lab is the first to combine them into a simple, inexpensive package that will be easy to deploy at the point of need, especially in developing regions where finger-prick blood sampling and the availability of trained medical personnel to diagnose samples may be challenging.
The hollow needles are 375 microns wide and 750 microns long, enough to reach the fluid within skin that is typically between 800 to 1,000 microns thick. The needles are sharp enough to overcome the mechanical stress of entering the skin.
“Xue and I have applied the patch to our skin, and it doesn’t feel painful at all compared to a finger prick or a blood draw,” Lillehoj said. “It’s less painful than getting a splinter. I would say it feels like putting tape on your skin and then peeling it off.”
They think the familiar form factor may provide some comfort, especially to children.
“We didn’t intend for it to look like a bandage,” he said. “We started with a rectangular shape and then just rounded the edges to make it a little more presentable. We didn’t plan for that, but perhaps it makes the patch more relatable to the general public.”
He estimated individual patches could cost about $1 if and when they are produced in bulk.