Using nanotechnology to help mRNA fight against COVID-19, a new approach to gene therapy could improve (Nanotechnology may improve cell therapy for blindness) how doctors treat hereditary blindness.
A team of researchers at Oregon Health & Science University and Oregon State University have developed a method that uses lipid nanoparticles – small balls made of fat – to deliver ribonucleic acid, or mRNA, into the eye. To cure blindness, mRNA must be modified to produce proteins that reverse vision-damaging gene mutations.

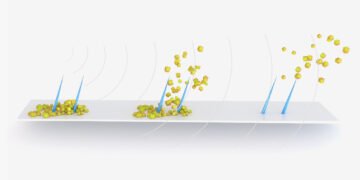
In a study published today in Science Advances, the team demonstrates how their lipid nanoparticle delivery system targets cells that are sensitive to light, called photoreceptors, in mice and humans not human. The system’s nanoparticles are coated with a peptide that researchers found to be attractive to photoreceptors.
“Our peptides are like postal codes, and lipid nanoparticles are like envelopes that send gene therapy by mail,” said the author of the study, Gaurav Sahay, Ph.D., associate professor in the OSU College of Pharmacy explained. who also has a joint research appointment with the OHSU Casey Eye Institute. “The peptide ensures that the mRNA is delivered specifically to the photoreceptors – cells that we have not been able to target with lipid nanoparticles until now.”
“More than 250 genetic mutations have been linked to inherited retinal diseases, but only one has a proven gene therapy,” said study author Renee Ryals, Ph.D., assistant professor of ophthalmology at the OHSU School of Medicine. of Medicine is added. scientist at the OHSU Casey Eye Institute. “Improved technology used for gene therapy may provide more treatment options to prevent blindness. The results of our study show that lipid nanoparticles can help us do that.

In 2017, the Food and Drug Administration approved the first gene therapy to treat hereditary blindness. Many patients have experienced better vision and avoided blindness after receiving the treatment, which is sold under the brand name Luxturna. It uses a modified form of adeno-associated virus, or AAV, to deliver gene-editing molecules.
Today’s gene therapies are based on AAV, but they have some limitations. This virus is small and cannot contain the genetic editing machinery for some complex mutations. In gene therapy AAV can only deliver DNA, leading to the creation of gene-editing genes that can lead to unexpected genetic changes.

LIPid nanoparticles are another promises that are worth it because they have no obstacles as AAV. In addition, LIPid nanoparticles can rescue the Mrna, which also controls a brief, so the changes may be blocked. The potential of lipid nanoparticles has been demonstrated by the success of mRNA-based COVID-19 vaccines, which also use lipid nanoparticles to deliver mRNA. They are also the first vaccines licensed for COVID-19 in the United States, due to the speed and volume with which they can be developed.
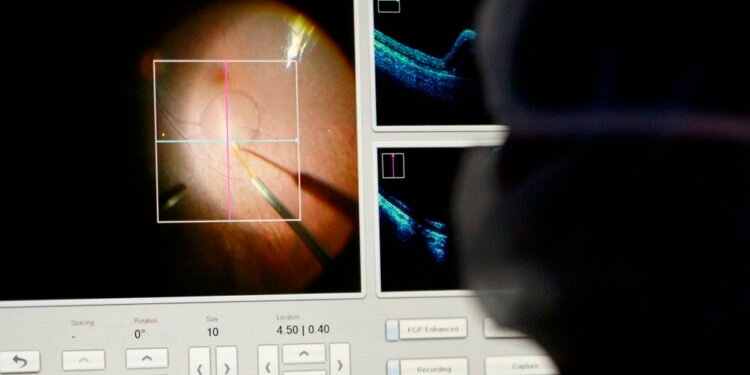
In this study, Sahay, Ryals and their colleagues showed that the envelope of lipid nanoparticles coated with peptides can be directed to photoreceptor cells in the retina, the tissue behind the eye that provides opportunity to see. As an early proof of concept, mRNA containing the instructions to make a green fluorescent protein was incorporated into the nanoparticles.
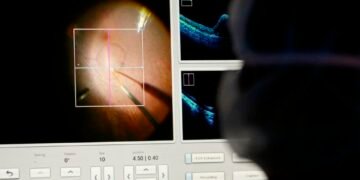
After spreading this nanoparticle gene therapy to the eyes of mice and non-human animals, the research team used different imaging techniques to examine the treated eyes. the retinal tissue glows green, indicating that the lipid nanoparticle shell reaches the photoreceptors and that the mRNA it delivers successfully enters the retina and produces green fluorescent protein. This research is the first known lipid nanoparticles to target photoreceptors in a non-human primate.
Scientists are currently working on observational studies to determine the amount of green fluorescent protein expressed in animal retinal models. They are also working on developing therapeutics on mRNA that carries the code for gene-editing genes.
Sahay and Ryals will continue to develop nanoparticle gene therapy delivery systems with the support of a new $3.1 grant from the National Eye Institute of the National Institutes of Health.