Scientists build human lungs in boxes to test drugs. This Small lungs can replace animal testing and improve the success of clinical trials.
The research will be published in Biomaterials Research available online in preprint form, led by Dr Huyen Phan of the University of Sydney and colleagues from Australia, South Korea and China.
Lab-engineered lungs, known as organoids or mini-organs, are 3D structures made from basic human cells that mimic the organs in the body. They serve as a test bed for biomedical research.
Lead author Professor Wojciech Chrzanowski, Professor of Nanomedicine at the Sydney School of Pharmacy, Faculty of Medicine and Charles Perkins Center Fellow said: ‘This work is important because we will be able to reduce the number of animals in medical research. and accelerate the discovery of new drugs or new strategies to treat diseases.
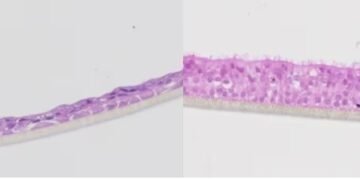
“We decided to build two different types of lungs, one of which mimics the process of a clinical trial; a healthy lung to study the safety of a new drug. The other mimics two parts of the trial; a diseased lung which, in our case, shows a chronic disease that prevents lung disease, allowing us to study the therapeutic effect or the superiority of medicine.
“We take cells directly from patients and build them up to the same level as they are in the body. So first you have epithelial cells, then you have fibroblasts – we create a mimetic organ that similar to a real human lung.
Professor Chrzanowski said the models described in the paper, which are more accurate than traditional models, are unique in their ability to mimic the environment of the human lung. AstraZeneca and the U.S. Food and Drug Administration are currently using the models.
“With traditional cell culture, you put cells in a petri dish and grow them under static conditions, which is a far cry from what happens in the human body. What we are doing is creating an environment similar to that of the human body,” said Dr Phan.
“We develop and maintain our species in the micro-environmental conditions of the lungs, with air on the one hand and liquid on the ground, connected to the microcirculation, which is our blood system or blood.”
“These two things together help to mimic the condition of the human lungs, making them better.”
The use of lung models is not isolated to medical research. They can be customized for each patient and used to test different reactions in the lungs.
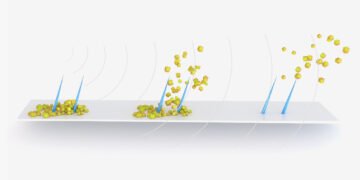
“Organoid models of small lungs can also be used to test for toxicity. For example, silica dust or air pollution, such as particles produced during forest fires,” said Professor Chrzanowski.
“Because we can extract cells directly from individual patients, we can create a patient model to test the effectiveness of drugs on them.”
Professor Chrzanowski said lung models could have a major impact on basic science, helping to determine how different organs work and how to develop the most effective treatment regimens.
The researchers say the biggest advantage of their models is their reproducibility, reliability, and ability to conduct large-scale research efficiently.
“They speed up the diagnostic process, they shorten the process of arriving at the hospital, and they significantly increase our confidence in the molecules we create before we proceed to clinical trials,” said Professor Chrzanowski.
“The time for clinical translation is about 10 to 15 years, but when you use the organoid model you can reduce that time significantly.”
The development of these types of lungs brings Australia to the forefront of organ research, said Professor Chrzanowski, who called for the creation of a national center for further medical research in animal methods.
Australia has banned cosmetic animal testing in 2020 and last year the United States introduced legislation ending the requirement to test new drugs on animals.
Source: The University of Sydney