Australian nanomedicine researchers have developed a new way to solve a decades-old clinical problem: getting therapeutic drugs to act selectively on cancer cells in the body, a Landmark in childhood cancer treatment.
Published this week in the high-impact journal Science Translational Medicine, the research points the way to safer and more effective treatments for children with aggressive blood cancers, as well as other types of cancer.
Chemotherapy is the main treatment for leukemia, a blood cancer most common in children. However, although chemotherapy can be effective for some types of leukemia, it is not effective for some other types, called ‘high-risk’ leukemias.
Treatment for high-risk leukemias often involves doses of drugs that flood the body, affecting both cancer cells and healthy cells. This often results in serious side effects, as well as life-long health problems in survivors.
“Finding ways to make chemotherapy drugs work more effectively on cancer cells is key to improving treatment progress and reducing toxicity in children being treated for leukemia. up,” Professor Maria Kavallaris AM, Director of Translational Cancer Nanomedicine in Pediatric Cancer Institute, who did the research. “By targeting leukemia cells specifically, we can make the treatment more effective and safer to use in children.”
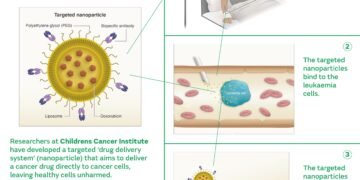
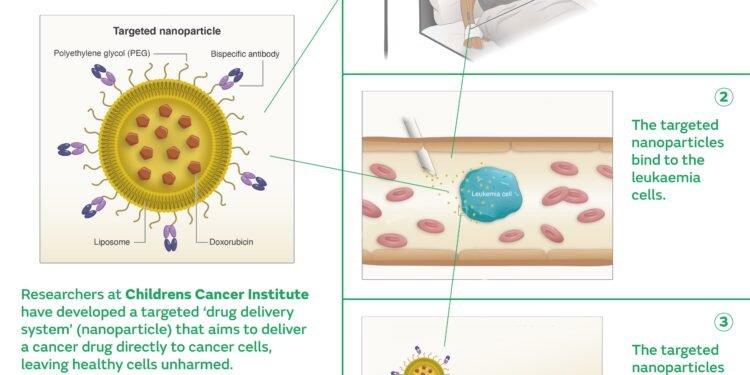
In a recently published study, scientists from the Children’s Cancer Center and collaborating organizations used a unique form of cancer drug, doxorubicin (Caelyx ), where the drug is encapsulated in particles called liposomes.
In this process, they added ‘bispecific antibodies’ – antibodies that can recognize and engage the drug at one end and the cancer cells at the other end, effectively acting as a bridge between the middle of the two. Known as the “targeted drug delivery system”, it works to deliver the drug to its target, in this case, leukemia cells, where the drug can do its job and kill the cells.
“What is particularly useful about this new approach is its flexibility,” said author Dr. Ernest Moles, a researcher at the Children’s Cancer Institute. “We can use this system to target any leukemia, including the high-risk subtypes that kill Australian children every year.
Instead of creating a completely new treatment every time, all we have to do is change the immune bridge, and we can apply the same drug to every child’s blood cancer.
“Furthermore, this system may prevent us from becoming resistant to individual drugs. If childhood cancer cells try to evade chemotherapy by changing their cell surface, we can modify the targeted drug delivery system so that it can recognize the changed cancer cell. Escape will not be easy.
Photos;
This new method has been shown to work well not only in growing leukemia cells, but also in live models of the disease. In these models, a targeted drug delivery system was found not only to reduce the number of leukemia, but also to prolong life – in some cases, up to four times.
The researchers believe that this same approach can be used to improve the selection of the next generation of chemotherapy, not just chemotherapy, paving the way to provide children with safer alternative treatment options than what is currently being offered.
They are also excited about the potential contribution to the emerging generation of precision medicine. “In the future, it may be that every child diagnosed with leukemia can have their treatment based on their subtype, based on the analysis of blood samples,” said Professor Kavallaris.
“We believe that the observation of controlled nanotherapies represents a positive step forward in the treatment of childhood cancer, and we are optimistic about what this can lead to.
Matt Weston and his son Jacob, who are currently being treated for acute lymphoblastic leukemia, know the importance of this research. Matt said, “This research project is well-followed, and I am blown away by the work of Maria, Ernest and the team at the Cancer Center.”
“Having already experienced the toxicity of chemotherapy during my son’s journey, I can tell you horror stories about the side effects, even with the risk assessment., but their chances of survival are also much lower.
“I think about these children and their families all the time, and knowing that we are on the cusp of improving treatment, reducing toxicity and improving their chances of survival gives me great hope.”
Jacob has already undergone chemotherapy for the past eight months and has had many debilitating side effects. But not yet, He still has 16 months of rehabilitation, but it will be another three years before he gets the green light, Matt said: “It will be a long way to go. You can read more about Jacob’s story here.