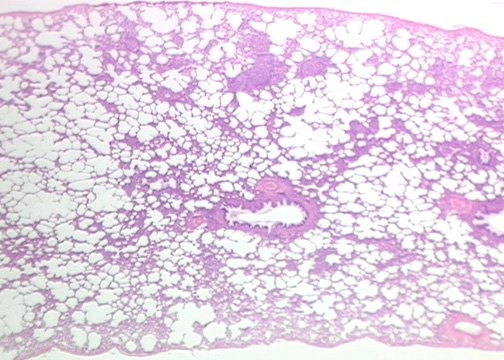
Lung tissue. Courtesy: Rutgers University
Scientists used human white blood cell membranes to carry two drugs, an antibiotic and an anti-inflammatory, directly to infected lungs in mice.
The nano-sized drug delivery method developed at Washington State University successfully treated both the bacterial growth and inflammation in the mice’s lungs. The study, recently published in Communications Biology, shows a potential new strategy for treating infectious diseases, including COVID-19.
“If a doctor simply gives two drugs to a patient, they don’t go directly to the lungs. They circulate in the whole body, so potentially there’s a lot of toxicity,” said Zhenjia Wang, the study’s corresponding author and an associate professor in WSU’s College of Pharmacy and Pharmaceutical Sciences. “Instead, we can load the two types of drugs into these vesicles that specifically target the lung inflammation.”
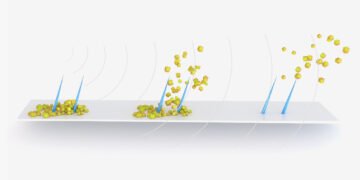
Wang and his research team have developed a method to essentially peel the membrane from neutrophils, the most common type of white blood cells that lead the body’s immune system response. Once emptied, these membranes can be used as nanovesicles, tiny empty sacks only 100 to 200 nanometers wide, which scientists can then fill with medicine.
These nanovesicles retain some of the properties of the original white blood cells, so when they are injected into a patient, they travel directly to the inflamed area just as the cells would normally, but these nanovesicles carry the medicines that the scientists implanted to attack the infection.
In this study, first author Jin Gao, a WSU research associate, loaded the nanovesicles with an antibiotic and resolvinD1, an anti-inflammatory derived from Omega 3 fatty acids, to treat lungs infected by P. aeruginosa, a common potentially fatal pathogen patients can catch in hospital settings. The researchers used two drugs because lung infections often create two problems, the infection itself and inflammation created by a strong immune system response.
Toxicity studies and clinical trials would have to be conducted before this method could be used in human patients, but this study provides evidence that the innovation works for lung inflammation. If the method is ultimately proven safe and effective for humans, Wang said the nanovesicles could be loaded with any type of drug to treat a range of infectious diseases, including COVID-19.
“I think it’s possible to translate this technology to help treat COVID-19,” said Wang. “COVID-19 is a virus, not a bacterial pathogen, but it also causes an inflammation response in the lung, so we could load an antiviral drug like remdesivir into the nanovesicle, and it would target that inflammation.”