Cancer treatment decisions may be better for individual patients using a new imaging (A new imaging technique of a tumor) technique developed by University of Michigan researchers that pinpoints the chemistry of a patient’s tumor.
Today, cancer treatment methods, whether surgery, radiotherapy or immunotherapy, are recommended, depending on the location, size and severity of the tumor. This information is generally obtained from anatomical images – MRI or tomography or ultrasound and biological tests performed on tissues obtained from tumor biopsies.
But the chemical environment of the tumor has a great influence on the effectiveness of a particular treatment. For example, a low level of oxygen in tumor tissue impairs the effectiveness of radiation therapy.
Now, a team of scientists from the University of Michigan and two Italian universities have demonstrated that an imaging system that uses special nanoparticles can provide a real-time, high-resolution chemical map that shows the distribution of chemicals from interest in a tumor.
This could lead to ways to help doctors make better recommendations about the right cancer treatment for a particular patient – precision medicine.
Their research, published in ACS Nano, reports the first demonstration of a common in vivo chemical imaging technique for any chemical of interest, according to UM chemistry professor Raoul Kopelman, one of the – guide the authors of this book.
The researchers used a technique of “chemical imaging” of the tissue called photo-acoustic chemical imaging, or PACI.
“What’s new about this method is that it’s done in vivo, right inside the body,” Kopelman said.
The team tested their method in mice transplanted with tissue from a patient’s tumor, called a xenograft. Patient-derived xenografts recapitulate the genetic and biological characteristics of the patient’s tumor.
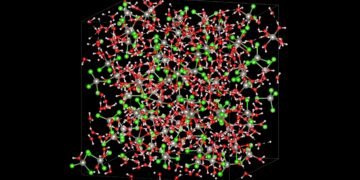
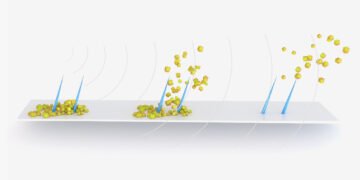
PACI uses nanoparticles developed over the past few decades by Kopelman and others that can be injected into mice to measure tumors and detect certain chemicals of biomedical interest, such as oxygen, sodium or is potassium.
When this nanosensor is activated by infrared laser light that can penetrate into the tumor tissue, an ultrasound signal is generated that can be used to determine the concentration and distribution of the chemical.
The PACI method can be used in mouse xenografts to evaluate the characteristics of a patient’s tumor repeatedly to monitor the chemical environment of the tumor over time.
“It will allow for the optimization of the treatment process for one patient, the right medicine,” said Kopelman.
Kopelman and his colleagues used PACI with a targeted nanoparticle to detect oxygen. After radiotherapy, the brain and mice, researchers found a significant correlation between oxygen levels in each part of the brain and how radiotherapy destroys tumor tissue – reducing oxygen in the tissue, reduces the effectiveness of local radiotherapy.
“Therefore, we provide a simple, non-invasive and inexpensive method to determine the effectiveness of radiation therapy for a given tumor and identify areas of resistance to treatment in the tumor microenvironment,” said Kopelman.
“Such a chemical map will help the clinical team to provide personalized and optimal treatment for the patient’s tumor, based on the new discovery of the chemical map of the tumor xenograft.”
In this study, PACI was used in patient-derived xenografts. The ultimate goal will be the ability to map chemicals directly to patients.
This is possible, says Kopelman, and the optical fiber will be taken from the venous system of the patient, as is done in the heart system, to get closer to the tumor. Nanosensors can be laser-activated, but this requires a nanosensor designed for each chemical of interest, and each nanosensor would need to be approved by the Food and Drug Administration.
Source: University of Michigan