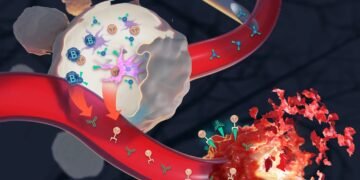
Vaccination as tumor therapy – with a vaccine made individually from a patient’s tissue sample that “glues” the body’s own immune system to (Cancer vaccination) cancer cells: the basis for this long-term panawon has now been obtained by a group of researchers from the MPI for Polymer Research and the University Medical Center Mainz, in particular from the Institute of Immunology and dermatology. Their results were recently published in the journal ACS Nano.
“We are introducing a new class of vaccines that can be an effective alternative to mRNA vaccines,” said Prof. Dr. Lutz Nuhn, until now group leader of Tanja Weil’s department at the MPI for polymer research and recently appointed professor of macromolecular chemistry at the Julius-Maximilians-University in Würzburg. This is important, for example, for people in whom the production of proteins in the body is disturbed during vaccination with the mRNA vaccine – i.e. those that are sometimes used against corona – and on which these vaccines have limited effect.
However, the main reason is that if cancer vaccines are to become routine one day, it is necessary to explore different effective strategies to provide important important information to specific immune cells.
Antigen plus immune activator – combined with nanoparticles
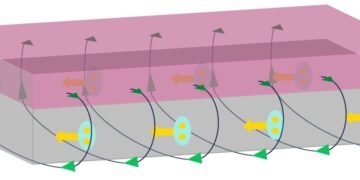
The new type of vaccine consists of two components: firstly, it is an antigen that is specific to the tumor cell and must be recognized by the immune system as an “enemy”, so to speak, and secondly, an immune activator – a “sting”. “It will shake the immune system.
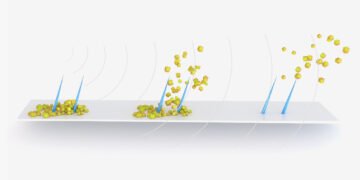
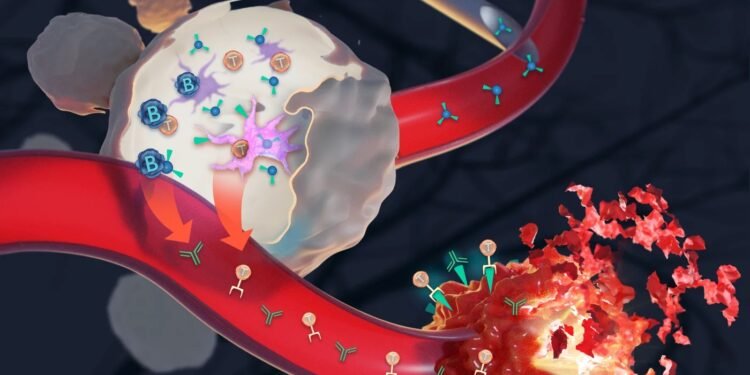
As an immune activator, scientists used a derivative of a chemical molecule discovered by Sunil A. David in the USA and successfully used in the Indian corona vaccine Covaxin. By itself, this molecule is very active and powerful and can cause severe inflammatory reactions throughout the body. Therefore, the research team included it in a carrier – more precisely, in polymer-based nanoparticles with a gel-like consistency, biodegradable and locally limiting the effect of the immune activator. These nanomaterials, with a diameter of less than 100 nanometers, are the same size as viruses – the cells of the immune system recognize them well, eat them and in this way wake up from sleep mode. Nanoparticles thus open a direct path to the immune system. A: “By attaching them to the nanopolymers, we were able to throttle the immune response to the desired level,” Nuhn explained.
The vaccine specifically kills tumor cells
For a vaccine to target a tumor, you need to know: What distinguishes tumor tissue from healthy tissue—in other words, what specific antigens are found in cancer? This may be patient specific. “When a tumor is diagnosed in the early stages, it’s a race against time to develop a patient-specific vaccine as quickly as possible,” Nuhn explained.
To develop new types of vaccines, scientists first use a model antigen. They develop various tumors that carry this model antigen – both on the surface and inside. Initial studies are promising; T cells activated by the vaccine only kill tumor cells that carry the antigen on their surface or even inside. Healthy tissue, on the other hand, is not affected. “The polymer-based nanocarrier is a useful tool to further investigate antigen-specific vaccines and to develop other vaccine-based cancer therapeutic concepts,” believes Nuhn. But one thing must be said: Many years of further research are needed before such vaccines can cure cancer patients. It is also not possible to prevent all types of cancer with a vaccine.