A team of scientists led by Xiling Shen, Ph.D., Chief Scientific Officer and Professor at the Terasaki Institute for Biomedical Innovation (TIBI), has reached a new level of development in a patient model. They developed (Expanding the possibilities of microorganospheres) better methods for generating microorganospheres (MOSs) and showed that these MOSs have excellent potential for various clinical applications.
As documented in a recent publication in Stem Cell Reports, their MOS can be used as patient avatars for studies that capture direct viral infection, immune cell penetration, and high-throughput screening of therapeutics not available in conventional patient models.
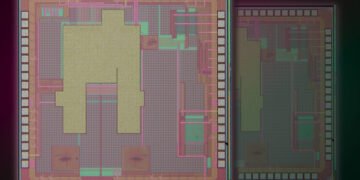
Team Dr. Shen has developed (Expanding the possibilities of microorganospheres) an emulsion microfluidic technology to produce MOS, nanoliter droplets of basement membrane extract (BME) composed of mixtures of tissue cells that can be generated at high speed from an automated device. After the droplets are formed, the excess oil is removed by a new membrane demulsification process, leaving behind thousands of viscous droplets of uniform size with a small 3D tissue structure.
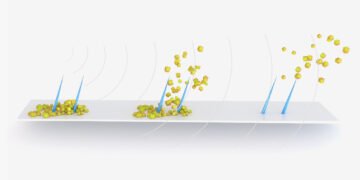
The team continues to demonstrate the unique capabilities and properties of the MOS in several first-class experiments. They were able to demonstrate that MOS can be generated from a variety of tissue sources, and the resulting MOS has the preservation of histopathological morphology, the ability to differentiate and genetic expression, and the ability to freeze and subculture, like conventional organoids. . Experiments were performed to test the ability of MOS to infect viruses. Unlike conventional organoids, MOS can be directly infected with viruses without removing and suspending cells from the surrounding BME scaffold, thereby restarting the viral infection process in the host tissue.
Dr. Shen’s team was able to create a MOS atlas of human respiratory and digestive tissues from patient autopsies and infect them with SARS-COV-2 viruses, followed by drug screening to identify drugs that block viral infection and replication within those tissues.
MOS also provide a unique platform for studying and developing immune cell therapy. Within natural diffusion limit of vascularized tissue, tumor-derived MOS allowed sufficient penetration by therapeutic immune T-cells such as CAR-T, enabling a novel T cell potency assay to assess tumor killing by the engineered T-cells. Such a model would be highly useful in investigating tumor responsiveness and in developing anti-tumor immune cell therapies.
MOS could be further integrated with deep-learning imaging analysis for rapid drug testing of small and heterogeneous clinical tumor biopsies. In addition, the algorithm can identify cytotoxic versus cytostatic drug effects and drug-resistant clones that may cause late relapse. This pioneering work paves the way for the use of MOS in the clinic to inform treatment decisions.
“Dr. Shen and his team continue to refine and develop the MOS technology, highlighting its versatility, not only as a physiological model for screening potential personalized treatments, but also for studying diseases and various applications,” Ali said. Khademhosseini, Ph. .D. , Director and CEO of TIBI. “This is the wave of the future in precision medicine.”